Disclaimer: This blog post solely reflects the opinion of the authors and should not be taken to represent the general views of IPPR’s management/ editorial team or those of fellow authors.
You think it can’t happen to you. Then, one day, your world is suddenly turned upside down by a life-threatening diagnosis. In the case of Brian Wallach, a US healthcare activist diagnosed with a rare form of sclerosis, healthcare funding could have saved his life. For thousands of kidney cancer patients in the UK, it could’ve prolonged their lives. None received funding. At its worst, this is a state-issued death sentence. At best, can it be the ethical choice of the lesser evil?
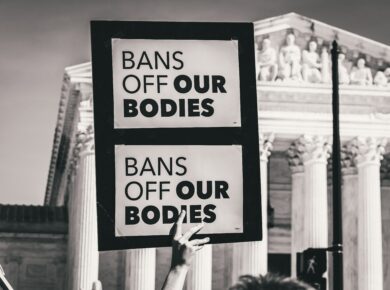
Source: Unsplash
https://tinyurl.com/2xx6d2dd
With the media debate largely centred around the US issue of whether to offer state healthcare at all, most countries with state-run healthcare systems are forgotten, and so is an essential question: to whom should governments provide it?
The obvious answer is everybody, ideally. However, the reality of scarce resources and shrinking budgets for non-COVID illnesses forces us to choose. Even in times of economic abundance, healthcare is so expensive that turning it into a freebie for everybody who needs it is impossible. As a result, all state-run systems limit the kind of treatments they fund in one way or another. Even Switzerland’s medical system, ranked world’s best in the last Euro Health Consumer Index, includes gatekeeping restrictions on certain treatments.
This means that some of us will pay taxes with the expectation of receiving the health benefits of the social contract and will be denied treatment when we need it. For most people, this is a hard pill to swallow. It forces the government to play God and us to accept elected officials’ criteria for who lives and who dies. Since some must be left behind, it’s worth looking at how the UK distributes treatments.
The UK’s utilitarian legacy: treating those who benefit most
Ranked 16th out of 35 on the Euro Health Consumer Index, the UK is part of a growing number of countries following the trend of treating those who will benefit most. To assess the benefit gained from treatment, they use a measurement called “quality-adjusted life years” (QALY).
To understand what QALY measures, we need to look at how it was created. Fundamentally, it is based on the idea of welfare economics, meaning that people’s preferences are best suited to determine the value of their own welfare. Large samples of the population were asked to ascribe values to different health states to determine the value of that state. Would you rather live 3 years in moderate pain or 1 year without pain?
After aggregating this data, prolonging life for different amounts of time for people with different conditions could be objectively compared through the QALY, or so the story goes. Then, the UK could set a cost-effectiveness threshold for funding only the most effective treatments at the lowest price. If your treatment is effective but highly costly, it would not be funded.
According to NICE (The National Institute for Health and Care Excellence), the UK’s body for deciding treatment funding, the reasoning is that you would be taking funding away from people who would benefit more from the same investment. While letting one suffer for the higher benefit of another might sound cruel, it can’t be accused of being inegalitarian.
Source: The auto-icon https://www.traveldarkly.com/jeremy-benthams-head-auto-icon-ucl-london/
At face value, this seems like a fair principle. Its application demonstrates that Bentham’s philosophy is far from resting with him in his wooden UCL box and that the UK governments’ evidence-based approach to politics is here to stay. Adopting “what works” is the ramification of Bentham’s brainchild and this Western political tradition doesn’t shy away from determining whether you get life-saving medicine.
What about those who need it the most?
NICE’s practices were heavily criticized by advocates of the worse-off, and rightfully so. Take this example. Your medicine could be life-saving, but someone else’s could significantly improve their life quality. If your treatment is more expensive, your life might be sacrificed in favour of bettering someone else’s. However significant the other person’s gain might be, it’s hard to make the argument that it trumps another’s life.
It turns out the public agrees. In a series of opinion polls, researchers found that public opinion values saving the lives of people who can not reach perfect health equally to restoring someone’s maximum health condition.
Thankfully, UK bureaucracy adapted to these preferences. Following long-term lobbying attempts and hearings, NICE implemented a series of exceptions to the cost-efficiency rule, including end of life situations and people with pre-existing disabilities whose health can not be restored to the standard maximum levels. It now decides whether treatment will be funded on a case-by-case basis considering cost-efficiency and potential exceptions.
Nobody to blame?
The UK health system tries to combine the efficient with the humane, but this is easier said than done. After refusing funding to kidney cancer patients due to extremely high costs, Dr Pat Hanlon, from Kidney Cancer UK, accused NICE of “robbing people of a few months of life”.
Denying anybody healthcare is set to produce some heart-breaking stories. But when you must rob somebody of something no matter what you choose, picking the ones that will truly benefit from funds while not leaving the sickest behind seems like the right option. While healthcare funding in the UK is far from perfect, with multiple accusations of NICE not living up to its own standards, the ethical considerations of those standards seem well-balanced.
By Nina Renata
Nina is in her second year of studying Politics and International Relations at UCL. Passionate about discovering the explanations behind the headlines and debating their intricacies, she is currently serving as IPPR’s Editor-in-Chief.