Disclaimer: This blog post solely reflects the opinion of the authors and should not be taken to represent the general views of IPPR’s management/ editorial team or those of fellow authors.
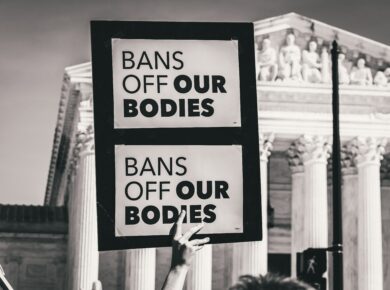
Too often, the medical system leaves women “misunderstood, mistreated and misdiagnosed” (Perez, 2020, p. 196). From data gaps found in research that translate to the same gaps in medical-school curriculums, to data gaps in pharmaceutical trials, which result in drugs that don’t work for women. Medicine has, for too long, functioned on the assumption that male bodies represent all human bodies, leading to disastrous consequences for half of the population.
Is there a sex-specific data gap in medical research?
The short answer is yes. One of the most well-known examples of this occurred in the 1970s. A drug called thalidomide had been available as an over-the-counter sedative when doctors began prescribing it to pregnant women as a solution to their morning-sickness. Although a dose high enough to kill a rat hadn’t been found, it proved to affect fetal development, something the manufacturers were aware of much earlier. As a result, over “10,000 children had been born around the world with thalidomide-related disabilities” (Perez, 2020, p. 201) by the time the drug was taken off the market in 1962. Following this, in 1977 FDA issued guidelines that exclude women of childbearing age from potential drug trials, resulting in the male body being accepted as the norm.
The acceptance of the male body as the norm accounts for why women continue to be excluded from research and medical trials. For example, between 1987 and 2012 women accounted for “25% of participants across thirty-one landmark trials for congestive heart failure” (Perez, 2020, p 200). However, the issue of exclusion stems from much deeper. Namely, the belief held by some researchers that biological sex doesn’t matter, despite all the evidence that it does. Furthermore, it is argued that female bodies are “too complex, too variable, too costly to be tested on” (Perez, 2020, p. 202) resulting in their exclusion on the basis of simplicity. In addition, it is also argued women are simply excluded as they are harder to recruit. This may be due to the fact that overwhelmingly the burden of care falls on women, and so they may simply be unavailable during the times the trials take place, or too busy to participate. However, this is not an adequate excuse to exclude roughly half the population from research and trials; the results of which will impact the treatments they receive from medical professionals. Instead, trial schedules could be adapted to make it possible for women to participate.
Why is the exclusion of women from medical research and trials concerning?
To begin, medical research informs how doctors are trained, and if there is no data pertaining to women, it’s no wonder they are misdiagnosed and mistreated. Throughout history, it has been assumed that the only fundamental differences between male and female bodies are in their size and reproductive organs and so medical education was focused on the male norm. However, this continues to be a problem in the present day. In 2008, an analysis of a range of textbooks recommended by twenty of the most prestigious universities found that “across 16329 images, male bodies were used three times as often as female bodies to illustrate neutral body parts”(Perez, 2020, p.197). In 2017 Caroline Criado Perez decided to see if anything had changed and unsurprisingly found that it hadn’t. Furthermore, it’s not only the textbooks themselves that lack information on women; it’s the medical curriculum itself. A review in 2016 found that “integration of sex- and gender-based medicine in US med schools remained minimal and haphazard [there were particular gaps in] the approach to the treatment of disease and use of drugs” (Perez, 2020, p.198). This also comes as no surprise as according to the FDA, “the second most common adverse drug reaction in women is that the drugs simply don’t work” (Perez, 2020, p. 204).
These gaps matter. Sex differences are real and meaningful. Sex differences have been discovered in every tissue and organ system in the human body (Keitt, 2004). There are also sex-differences in the fundamental mechanical working of the heart (Blair, 2006) alongside many other organs in the human body. A fundamental aspect not considered in drug trials which include women is their menstrual cycle. If women are included, they are in the early phase of their cycle when hormone levels are at their lowest, which happens when their bodies are functioning most similarly to men. Excluding women at different stages of their cycle excludes learning about how different medicines interact with the varying levels of hormones in a woman’s body. It is possible that a certain dose of a drug can be too little at a point in the cycle and too much at another point. This brings us back to women being mistreated by their doctors as a result of ingrained biases in the medical system.
What can be done to avoid misunderstanding, mistreating and misdiagnosing women?
The solution is quite simple. It all starts with listening to and believing women when they tell their doctors something is wrong. After all, the pain they feel is real and a better indicator of medical issues than what can be seen from the outside. Especially when considering women may experience different symptoms than men. For example, in a woman a heart attack may present with “stomach pain, breathlessness, nausea and fatigue” (Perez, 2020, p.218) and so go misdiagnosed because it doesn’t present with usual chest pain associated with a heart attack. It is also crucial to include women of different ages, at different stages in their menstrual cycle and most importantly, to sex-disaggregate the data. It is about time to stop denying the existence of sex-based differences and start asking what can be done to make drugs and treatments useful for the whole population.
References
Blair L.M., (2006). Sex-based differences in physiology: what should we teach in the medical curriculum? Advances in Physiology education 31(1) 23-25. Retrieved March 7, 2021, from https://journals.physiology.org/doi/full/10.1152/advan.00118.2006 ;
Keitt, S., Fagan, T., & Marts, S. (2004). Understanding Sex Differences in Environmental Health: A Thought Leaders’ Roundtable. Environmental Health Perspectives, 112(5), 604-609. Retrieved March 7, 2021, from http://www.jstor.org/stable/3838011 ;
Perez, C. C. (2020). Chapter 10: The Dugs Don’t Work. In Invisible Women : Exposing Data Bias in a World Designed for Men (pp. 195-216). London: Vintage.
By Ieva Sturina
Ieva is a first year Philosophy, Politics and Economics student passionate about cultural issues, sustainability and international relations.